Conditions We Treat
Osteoporosis and osteopenia (low bone mass) can occur in men. Some risk factors include a previous fracture, smoking, alcohol consumption, various medications (steroids/prednisone), and rheumatoid arthritis. Dr. Godhwani offers treatments to prevent osteoporosis-related fractures and complications while delivering individual care plans for his patients.
Arthritis
Arthritis affects one in five Americans and can make everyday life a pain. At Island Rheumatology and Osteoporosis, we have dedicated our work to making sure that arthritis and other autoimmune disorders don’t drastically impact your everyday life.
The doctors and staff at Island Rheumatology and Osteoporosis have the experience and passion for testing, diagnosing, and treating your arthritis symptoms, from dermatomyositis to vasculitis.
FACTS ABOUT ARTHRITIS
Arthritis is inflammation of one or more of your joints. Osteoarthritis and Rheumatoid are the two most common types of arthritis. Below are common symptoms of arthritis that you should be aware of:
- Joint Pain
- Joint Stiffness
- Swelling and/or Tenderness of a Joint
- Difficulty Moving a Joint
- Redness Around a Joint
HOW OUR TEAM CAN HELP WITH ARTHRITIS
 Our experts at Island Rheumatology and Osteoporosis also treat rheumatologic conditions such as:
Our experts at Island Rheumatology and Osteoporosis also treat rheumatologic conditions such as:
- Dermatomyositis
- Gout and Pseudogout
- Lupus-Related Skin Diseases
- Osteoarthritis
- Osteoporosis
- Polymyositis
- Raynaud’s Syndrome
- Rheumatoid Arthritis
- Regional Musculoskeletal Syndromes
- Reiter’s Syndrome or Reactive Arthritis
- Sjogren’s Syndrome
- Spondylitis and Ankylosing Spondylitis
- Temporal Arteritis
- Vasculitis
Osteoporosis
Osteoporosis is a silent skeletal disorder that results from a loss of bone mass, which affects men and women. The change in the structure of bones causes weakness and results in an increased risk of fracture. The most common fractures occur in the spine, wrist, and hip. Spine and hip fractures, in particular, may lead to chronic (long-term) pain, disability, and even death. Fortunately, you can take steps to reduce your risk of osteoporosis and avoid the often-disabling broken bones (fractures) that can result from this condition. If you already have osteoporosis, new medications are available to slow or even stop the bones from getting weaker. These medicines also can decrease the chance of having a fracture.
What causes osteoporosis?
Osteoporosis results from a loss of bone mass (measured as bone density) and a change in bone structure. Many factors raise the risk of developing osteoporosis and breaking a bone. You can change some of these risk factors but not others. Recognizing your risk factors is important so you can take steps to prevent this condition or treat it before it becomes worse.
Major risk factors that you cannot change include:
- Older age (starting in the mid-30s but more likely with advancing age)
- Non-Hispanic white or Asian ethnic background
- Small bone structure
- Family history of osteoporosis or an osteoporosis-related fracture in a parent or sibling
- Prior fracture due to a low-level injury, particularly after age 50
Risk factors that you may be able to change include:
- Low levels of sex hormones, mainly estrogen, in women (e.g., menopause)
- The eating disorders anorexia nervosa and bulimia
- Cigarette smoking
- Alcohol abuse
- Low calcium and vitamin D, from low intake in your diet or inadequate absorption in your gut
- Sedentary (inactive) lifestyle or immobility
- Certain medications, including the following:
- Glucocorticoid medications (also called corticosteroids), such as prednisone (brand names: Deltasone, Orasone, etc.) or prednisolone (Prelone)
- Excess thyroid hormone replacement in those taking medications for low thyroid or hypothyroidism
- Heparin, a commonly used blood thinner
- Some treatments that deplete sex hormones, such as anastrozole (Arimidex) and letrozole (Femara) to treat breast cancer or leuprorelin (Lupron) to treat prostate cancer and other health problems
- Diseases that can affect bones
- Endocrine (hormone) diseases (hyperthyroidism, hyperparathyroidism, Cushing’s disease, etc.)
- Inflammatory arthritis (rheumatoid arthritis, ankylosing spondylitis, etc.)
What Is Osteoporosis?
Osteoporosis is more common in older women, mainly non-Hispanic white and Asian women. Yet it can occur at any age, in men, women, and in all ethnic groups. People over age 50 are at the greatest risk of developing osteoporosis and having related fractures. Over age 50, one in two women and one in six men will suffer an osteoporosis-related fracture at some point in their lives. In the U.S., about 4.5 million women and 0.8 million men over the age of 50 have osteoporosis, according to 2005–06 data. These figures are lower than older estimates, suggesting that osteoporosis is decreasing in the population. This is consistent with recent trends seen as decreasing.
However, another 22.7 million women and 11.8 million men over age 50 have low bone mass (known as osteopenia). People with low bone mass are also at higher risk of fractures, but it is not as high as for people with osteoporosis. If bone loss continues, people with osteopenia can become osteoporotic.
How is osteoporosis diagnosed?
You can learn if you have osteoporosis by having a simple test that measures bone mineral density—sometimes called BMD. Dual-energy X-ray absorptiometry (DEXA) is the current best test for measuring BMD.
The test is quick and painless. It is similar to an X-ray but uses much less radiation. Even so, pregnant women should not have this test to avoid any risk of harming the fetus. DXA test results are scored compared with the BMD of young, healthy people.
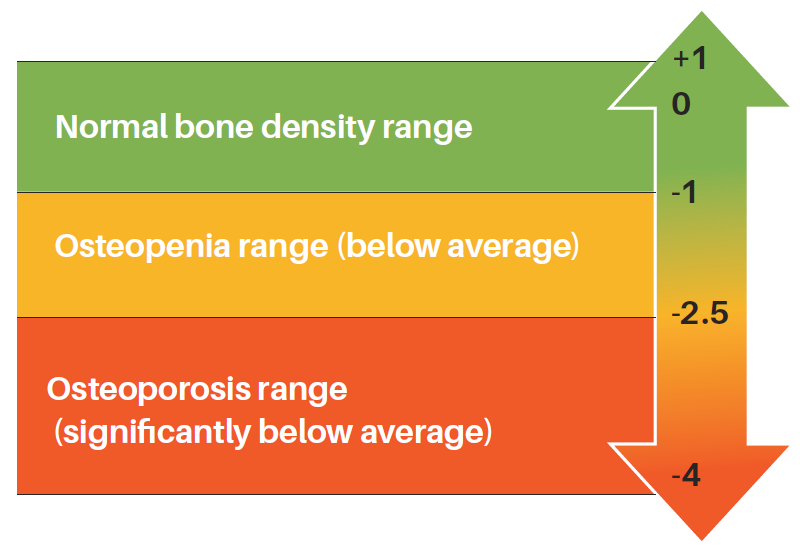
What's your T-Score?
Treatment
If you have osteoporosis, your healthcare provider will advise the following:
Calcium. Ensure you get enough calcium in your diet, or consider taking supplements. The National Osteoporosis Foundation recommends 1,000 milligrams (shortened as mg) per day for most adults and 1,200 mg per day for women over 50 or men over 70.
Vitamin D. Get adequate amounts of vitamin D, essential to help your body absorb calcium from the foods you eat. The recommended daily dose is 400–800 International Units (called IU) for adults younger than age 50, and 800–1,000 IU for those age 50 and older. (These are the current guidelines from the National Osteoporosis Foundation.) You may need a different dose depending on your blood level of vitamin D.
Physical activity. Get exercise most days, especially weight-bearing exercise, such as walking.
Some people also will need medication. Several medications are available for osteoporosis prevention and treatment (“management”).
Bisphosphonates are a class of antiresorptive drugs approved by the FDA for the management of osteoporosis. They are taken orally or intravenously and have been shown to slow down bone loss and decrease the risk of fracture. There are various side effects of orally taken medication, and they often have to be taken on an empty stomach with plenty of water. They may irritate the esophagus, and you have to remain upright for at least an hour after taking the medications. Rare side effects linked to bisphosphonates have been observed, such as osteonecrosis of the jaw (ONJ) and atypical femoral fractures.
Other medications include Teriparatide (Forteo), Denosumab (Prolia), Calcitonin, Estrogen or hormone replacement therapy, Selective estrogen receptor modulators, and others available for the management of osteoporosis.
Prevention
Lifestyle changes may be the best way of preventing osteoporosis. Here are some tips:
- Make sure you get enough calcium in your diet or through supplements (roughly 1,000–1,200 mg/day, but it will depend on your age).
- Get enough vitamin D (400–1,000 IU/day, depending on your age and your blood level of vitamin D measured by your doctor).
- Stop smoking.
- Avoid excess alcohol intake: no more than two or three drinks a day.
- Be physically active and do weight-bearing exercises, like walking, most days each week. Aim for at least 2½ hours a week (30 minutes a day, five times a week, or 50 minutes a day, three times a week), or as much as you can. Exercises that can improve balance, such as Tai Chi or yoga, may help prevent falls.
- Change lifestyle choices that raise your risk of osteoporosis.
- Implement strategies to help decrease your risk of falling.
You should also get treatment for any underlying medical problem that can cause osteoporosis. If you are taking a medication that can cause osteoporosis, ask your doctor if you can lower the dose or take another type of medicine. Never change the dose or stop taking any medicine without speaking to your doctor first.
If you have low bone density and a high risk of breaking a bone, your doctor may suggest medicine to prevent your bones from getting weaker. Healthcare providers now have a tool for estimating the risk of a patient’s osteoporotic fracture in the next ten years called the fracture risk assessment tool (FRAX). The World Health Organization developed it, and the score can help guide treatment decisions.
Rheumatologists are doctors who are experts in diagnosing and treating diseases of the joints, muscles, and bones. They can help find the cause of osteoporosis and provide and monitor the best treatments for this condition.
The most severe health consequence of osteoporosis is a fracture. Spine and hip fractures, especially, may lead to chronic pain, long-term disability, and even death.
The main goal of treating osteoporosis is to prevent fractures. If you have osteoporosis, it is essential to help prevent further bone loss and a fracture.
Here are some ways to decrease your chance of falls:
- Use a walking aid. If you are unsteady, use a cane or walker.
- Remove hazards in the home. Remove throw rugs. Also, remove or secure loose wires or cables that may make you trip. Add night lights in the hallways leading to the bathroom. Install grab bars in the bathroom and non-skid mats near sinks and the tub.
- Get help carrying or lifting heavy items. If you are not careful, you could fall or even suffer a spine fracture without falling.
- Wear sturdy shoes with soles that grip. This is true in winter or when it rains.
For more information:
National Osteoporosis Foundation – www.nof.org
International Osteoporosis Foundation – www.iofbonehealth.org


